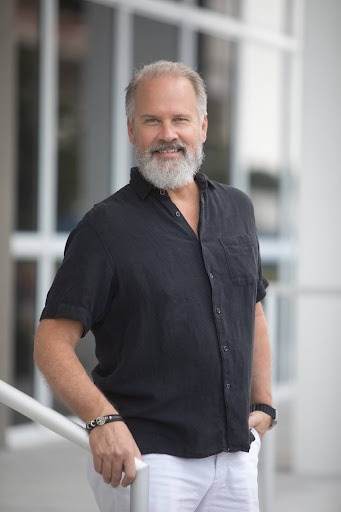
This article distills the insights and practical guidance shared by Chris Davenport, CISSP, CCSK, Allegrow’s Global Data Security Advisor and Fractional CISO. With more than 25 years of experience spanning community health systems, federal agencies, and global enterprises, Chris outlines why cybersecurity is now a CEO-level issue, why healthcare remains a “target-rich environment,” and what leaders can do right now to reduce risk without slowing growth.
The guidance that follows combines governance, risk, compliance, culture, technical controls, M&A due diligence, and the emerging threat landscape driven by artificial intelligence. It is presented as an actionable playbook: clear steps, checklists, and scorecard ideas leaders can use to evaluate readiness and prioritize the highest-impact activities this quarter and over the next 90 days.
Why Cybersecurity Is No Longer Just an IT Problem
Chris’s central message is straightforward: information security should not be treated as a back-office IT function. It is a cross-organizational responsibility that touches governance, operations, finance, legal, clinical care, and the boardroom.
He frames the problem this way: information security is like air conditioning; nobody notices it until it fails. When systems are working, security is invisible. When systems fail, the entire organization feels the heat. That is why leaders must understand security as an enterprise risk management problem, not simply a technical one.
At the heart of this approach are three interlocking domains:
- Governance: Policies, roles, and accountability, including who is responsible for what and how decisions are escalated.
- Risk Management: A repeatable framework to identify, classify, and mitigate the highest risks to operations and patient safety.
- Compliance: Meeting HIPAA, state regulations, NIST, and SOC requirements to avoid regulatory action and reputational damage.
When these domains are integrated, the organization can prioritize investments and make decisions that balance security with growth and clinical mission.
Why Healthcare Remains a Target-Rich Environment
Healthcare has become one of the most attractive targets for attackers. Chris outlines the main reasons:
- High-value data: Patient records contain names, addresses, Social Security numbers, insurance, payment information, and detailed medical histories, the kinds of information that are extremely valuable on illicit markets.
- Legacy systems: Many clinical systems were designed long before today’s threat landscape and are expensive or complex to replace.
- Underfunded IT: Budget constraints often leave security gaps, deferred patching, and limited staffing for monitoring and incident response.
- Complex device ecosystem: The Internet of Medical Things (IoMT) encompasses a wide range of medical devices, including MRIs, ventilators, infusion pumps, and EEG machines, each with its own software and connectivity requirements.
- Human factor: Healthcare workers are naturally inclined to help. Attackers exploit that willingness through social engineering and spear-phishing.
Put together, these features create a “target-rich” landscape where adversaries can use a variety of attack paths, phishing, credential theft and stuffing, vulnerable remote-access systems, third-party vendor access, and ransomware, to reach high-value assets.
Five High-Impact Actions to Take This Quarter
If an organization can do only five things this quarter, Chris recommends focusing on governance, risk, and foundational controls. The following list is prioritized to deliver the greatest reduction in risk for a limited time and budget.
- Establish or strengthen a GRC (Governance, Risk, Compliance) framework.
Define roles and accountability: who owns security at the executive level, who is accountable at the board level, and how decisions will be made. Develop or update key policies such as acceptable use, access control, incident response, data classification, and vendor management. - Perform a focused risk assessment and data criticality analysis.
Identify where patient data is created, received, maintained, or transmitted. Map the most critical assets and attack vectors. Classify risks as high/medium/low using a simple model: asset, attack vector, and likelihood/impact (Chris likens this to fire: remove one component and the risk is mitigated). - Prioritize a short list of technical controls.
Begin with multi-factor authentication (MFA), endpoint detection and response (EDR), network segmentation for critical systems, automated patching where possible, and secure backups that are regularly tested. - Kick off a practical, repeatable training program to build human firewalls.
Focus on phishing simulations, role-based training for privileged users, and operational awareness for clinicians. Use gamification and incentives to improve participation and retention. Remember that training without practical policies and enforcement weakens effectiveness. - Establish incident response and recovery planning, and run a tabletop exercise.
Ensure the organization knows how it will react to a breach that affects clinical systems. Include legal, communications, clinical leadership, and third-party vendors in exercises. Make sure backups are isolated and recovery times are realistic.
These five actions create a foundation: clarify responsibilities, know what matters most, harden the most exposed points, empower people to detect threats, and practice recovery.
Impacts of a Breach Beyond the Dollars
Financial losses from a breach are only part of the story. Chris highlights three other impacts that can far outlast associated remediation costs.
Patient Safety and Clinical Continuity
In modern healthcare, clinicians increasingly rely on electronic records, decision support systems, and connected devices. An outage can delay or interrupt care delivery, compromising timeliness and patient outcomes. In high-acuity scenarios like surgery or intensive care, the consequences can be severe.
Chris stresses that information access is central: “If you don’t know where your patient information is, your crown jewels, you’re going to have a hard time defending it.” Clinical teams need uninterrupted access to accurate information to treat patients effectively.
Legal and Regulatory Exposure
Breach notification laws, HIPAA enforcement from the Office for Civil Rights (OCR), and state-level regulations can result in investigations, fines, corrective action plans, and legal settlements. The OCR publishes high-profile enforcement actions that can tarnish institutional credibility.
Noncompliance also increases insurance premiums and complicates third-party relationships. The regulatory response is not just punitive; it requires remediation, audits, and sustained monitoring that consume operational resources.
Reputation and Trust
Reputation is often the most devastating casualty. The organization’s standing in the community, as a center of excellence, a trusted clinic, or a university hospital, can be damaged by public disclosures of a breach or ransomware attack. Loss of trust may lead to patient attrition, employee turnover, and difficulty recruiting clinical staff.
Chris notes that for many institutions, reputation ranks above the immediate financial loss. Protecting patient trust is therefore a strategic imperative.
Building a Security Culture that Sticks
Technical controls are necessary but insufficient. Lasting security relies on culture, a shared set of behaviors and expectations that starts with the board and the CEO and reaches the front line.
Start with Policies and Procedures
Chris considers policies and procedures the cornerstone of any security program. When board members and executives ask technical questions, the first response should be: “What does our policy say?” Policies convert ad hoc decisions into repeatable, auditable processes.
Human Firewalls: Training with Purpose
Effective training programs go beyond generic modules. They are:
- Role-specific: Clinicians, finance, HR, and IT have different threat profiles.
- Simulated and measured: Phishing simulations and response metrics identify gaps.
- Engaging: Gamification, low-cost giveaways, and positive reinforcement increase participation.
- Practical: Teach simple, repeatable actions (e.g., verify requests for fund transfers, never share credentials, and carefully handle removable media).
Chris suggests creative touches to make training memorable: “I’ve seen very successful training sessions where they’ll hand out toothbrushes and say, ‘Don’t share your toothbrush, don’t share your password.’” These memorable metaphors help turn abstract policies into everyday practice.
Incentivize and Empower Staff
Create channels for staff to report suspicious activity without fear of blame. Reward timely reporting and celebrate examples where vigilance prevented an incident. Turn security into a shared mission aligned with patient safety rather than a compliance burden.
Mergers & Acquisitions: Due Diligence Red Flags
M&A activity introduces significant integration risk. Chris has participated in multiple transactions and identifies practical signs that should trigger concern during due diligence.
Key Red Flags
- Disparity in security maturity: If one organization has mature policies, controls, and staff while the other treats security as an afterthought, the acquirer inherits risk.
- Old or orphaned vendor accounts: Directory services often retain stale vendor accounts that can be exploited to pivot into critical systems.
- Poor asset inventories: If the target cannot account for where patient data lives, the acquiring organization will face unknown liabilities.
- Inconsistent access controls and logging: Lack of centralized logging, weak authentication, or broad administrative privileges increases post-acquisition remediation costs.
Chris emphasizes that risk transfers with an acquisition. If the acquired entity suffers a breach, the parent organization bears the financial, operational, and reputational fallout.
AI and the Changing Attack Surface
Artificial intelligence is reshaping both defensive and offensive cyber capabilities. Chris warns that AI will accelerate attacker sophistication and scale.
AI-Powered Attacks to Watch
- Hyper-personalized social engineering: Attackers can scrape public sources and craft tailored phishing emails that bypass traditional red flags.
- Deepfake-based fraud: Audio and video deepfakes have already been used to impersonate executives and authorize fraudulent transactions.
- Automated malware generation: AI can generate polymorphic malware and streamline development, lowering the barrier to entry for adversaries.
- Credential stuffing and reconnaissance at scale: AI accelerates scanning and exploitation, enabling the rapid discovery of vulnerabilities.
These advances make social engineering more believable and technical exploits more accessible to less skilled attackers. Defenders must therefore rely more on fundamentals: the principle of least privilege, robust identity controls, and multi-layered monitoring capable of spotting anomalies that ML/AI-driven attacks create.
Rationalizing HIPAA, NIST CSF, and SOC Readiness
Healthcare leaders are often confused about how to rightsize a program that meets HIPAA requirements while aligning with frameworks like NIST CSF and achieving SOC readiness. Chris recommends a pragmatic approach: start with an assessment, prioritize based on risk, then implement a simple scorecard.
Assessment First
An assessment validates policies, interviews stakeholders, and examines system interconnections. It should answer:
- Where is patient data created, stored, and transmitted?
- What systems connect to each other and to the internet?
- Who has privileged access and how is it controlled?
- What logging, monitoring, and backups are in place?
The data criticality analysis is fundamental because “if you can’t define it, you can’t defend it.”
Example Simple Scorecard
A concise, executive-friendly dashboard can help leaders track progress and make decisions. Suggested components:
- Top Risks (3–5): Short descriptions with impact and mitigation status.
- Control Status: MFA coverage (% of accounts), EDR deployment (%), patch compliance (% of critical patches applied within SLA).
- Incident Metrics: Number of phishing clicks, mean time to detect (MTTD), mean time to respond (MTTR).
- Compliance Gaps: HIPAA-required policies are missing, NIST CSF categories are unaddressed, and SOC readiness items are incomplete.
- Third-Party Risk: % of vendors with security assessments, number of vendors with access to PHI.
- Recovery Readiness: Backup integrity (date of last test), RTO/RPO for critical systems.
Keep the dashboard lean and updated monthly. The goal is to provide executives and the board with a snapshot that supports informed, prioritized decisions.
Vendor and Supply Chain Risk: Controlling the Backdoor
Attackers increasingly exploit third-party vendors as an entry point. Chris outlines steps to reduce supply chain exposure.
Vendor Risk Management Practices
- Inventory and classify vendors: Identify which vendors have access to PHI or administrative systems.
- Contractual security requirements: Include data protection clauses, breach notification timelines, and audit rights in contracts.
- Least privilege and time-bound access: Limit vendor access to the minimum required and revoke accounts promptly after work is completed.
- Periodic security assessments: Require self-assessments, attestations, or independent audits (e.g., SOC 2 reports) based on vendor criticality.
- Continuous monitoring: Monitor third-party activity via logging and SIEM integration where feasible.
Failure to manage third-party risk can allow attackers to pivot from a single compromised vendor account into high-value clinical systems.
Incident Response, Backup, and Recovery Best Practices
Every organization must prepare for the inevitability of incidents. Chris stresses that recovery planning deserves equal weight with prevention.
Incident Response Essentials
- Define roles: Incident Commander, communications lead, clinical continuity lead, legal, and liaison to law enforcement.
- Run regular tabletop exercises: Include vendor and contractor representatives and realistic clinical scenarios.
- Maintain an escalation ladder: Clear thresholds for when to involve executives, regulators, and public communications.
- Forensic readiness: Ensure logs are retained in a tamper-evident manner for investigations.
Backup and Recovery Recommendations
- Isolate backups from production: Ensure backups cannot be encrypted or destroyed by the same attack.
- Test recovery frequently: Recovery tests should be realistic and time-bound to validate RTO/RPO assumptions.
- Maintain offline or immutable backups: Use immutable storage or air-gapped backups where appropriate for critical data.
- Document recovery runbooks: Clinical continuity playbooks for when electronic systems are unavailable (paper fallback).
Chris reminds leaders that recovery is not just a technical exercise but a clinical one: how will care continue when systems are down?
How Allegrow Engages: From Coffee Conversations to Action Plans
When organizations engage Allegrow, Chris describes the engagement model as intentionally pragmatic and collaborative.
Initial Conversation
The first step is a simple “coffee conversation.” Allegrow seeks to understand the organization’s current state, operating environment, systems in use, number of sites and employees, and the areas of concern, administrative, technical, or physical.
Assessment and Roadmap
If an assessment is warranted, Allegrow will evaluate policies, processes, system connections, and data flows. The result is a prioritized roadmap: an actionable 90-day plan that addresses top risks and prepares the organization for HIPAA, NIST, or SOC audits as needed.
Fractional CISO and Ongoing Support
For organizations without an internal CISO, Allegrow offers fractional CISO support: ongoing advisory services that provide strategy, governance, and program management at a fraction of the cost of a full-time hire.
Engagements can include SOC readiness support, HIPAA program development, vendor management systems, incident response planning, training programs, and continuous risk monitoring.
The Biggest Blind Spots Executive Teams Overlook
Chris points to three recurring blind spots he sees on executive teams and boards:
- Time constraints: Executives are pulled in many directions, and security can be deprioritized until an incident occurs.
- Competing priorities: With tight budgets and operational demands, security initiatives may be postponed in favor of clinical or revenue-generating projects.
- Resource limitations: Many healthcare providers simply lack sufficient budget or staff to maintain robust security programs.
To overcome these blind spots: make security a measurable part of the organizational strategy, present options scaled to the organization’s maturity and resources, and consider fractional expertise to fill capability gaps without large fixed expenses.
Practical Readiness Checklist: A 90-Day Starter Plan
This checklist condenses the earlier advice into a concrete 90-day plan for organizations that want to make measurable progress quickly.
- Week 1–2: Executive Alignment
- Hold a board/leadership briefing to agree on security priorities and assign an executive sponsor.
- Appoint an internal risk owner and define the governance cadence.
- Week 2–4: Assessment & Rapid Inventory
- Conduct a focused assessment: top clinical systems, data flows, and vendor access points.
- Perform a data criticality analysis to identify crown-jewel assets.
- Month 2: Immediate Controls
- Deploy or enforce MFA for all administrative and remote-access accounts.
- Roll out EDR to critical endpoints if not already in place.
- Validate backup isolation and schedule a recovery test for at least one critical system.
- Month 2–3: People & Policies
- Publish or update core policies (incident response, access control, data classification).
- Launch role-based phishing simulations and training with gamified incentives.
- Month 3: Vendor & M&A Checks
- Prioritize vendors with access to PHI for security assessments or SOC 2 reports.
- Close out stale vendor accounts from the directory services.
- End of 90 days: Executive Scorecard
- Deliver a one-page dashboard that includes the top three risks, MFA coverage, EDR deployment, backup test status, phishing click rate, and top remediation items.
- Present an actionable 6–12 month roadmap tied to budget and staffing recommendations.
Sample Executive Scorecard Metrics
A compact scorecard helps executives make decisions without getting lost in technical detail. Suggested items:
- Top 3 enterprise risks and current mitigation status.
- MFA coverage: % of users with enforced MFA.
- Patch compliance: % of critical patches applied within SLA.
- EDR coverage: % of critical endpoints protected.
- Phishing test click rate: baseline and targeted reduction.
- Mean time to detect (MTTD) and mean time to respond (MTTR).
- Backup test: date and outcome; RTO/RPO alignment with clinical needs.
- Vendor risk: % of critical vendors with up-to-date assessments.
What Leaders Can Learn from a Career in Data Security
Chris’s career spans banking, medical practice management, hospitals, global consulting, and international engagements. One recurring lesson he emphasizes is the importance of soft skills for security leaders.
He recommends Dale Carnegie’s classic, How to Win Friends and Influence People, to develop the interpersonal skills needed to translate technical priorities into board-level decisions and to work effectively across clinical and administrative teams. Good security programs are people-first: “If you got good people who are looking out after your organization and you know how to work with them, they’re going to be your best line of defense.”
Final Takeaways for Healthcare Executives
Chris leaves healthcare leaders with a clear call to action:
- Be proactive. Don’t wait to be blindsided by an incident.
- Prioritize risk management as a core executive responsibility.
- Begin by establishing policies, making small investments in high-leverage controls, and fostering a people-centered culture.
- Use assessments and scorecards to make informed trade-offs that protect patients, operations, and reputation.
Security is not a one-time project; it is an ongoing program aligned with clinical imperatives. Leaders who treat information security as integral to their mission will better safeguard patients and sustain trust in a digital healthcare environment.
FAQs
Q: Why should a CEO personally care about cybersecurity?
A: Cybersecurity is enterprise risk management. Major breaches affect operational continuity, patient safety, regulatory exposure, and organizational reputation. The CEO is accountable for protecting the institution’s mission, which now includes digital assets and patient data. Treating security as a board-level priority ensures resources, governance, and executive accountability.
Q: What are the most effective technical controls to implement quickly?
A: Start with measures that provide a high return on investment: enforced multi-factor authentication (MFA), endpoint detection and response (EDR), secure and tested backups, automated patch management for critical systems, and network segmentation for sensitive clinical devices. These controls dramatically reduce common attack vectors.
Q: How can a small medical practice rightsize a security program?
A: Small practices should focus on the essentials: a simple written policy set (data handling, breach response), MFA for email and administrative access, basic endpoint protection, offsite/immutable backups, and phishing-aware training. Use a compact GRC approach and consider managed or fractional security services to access expertise without hiring full-time staff.
Q: What should be included in M&A cybersecurity due diligence?
A: At minimum, assess the target’s policies, asset inventories, access control practices, vendor relationships, and recent security incidents. Verify whether system logs and backups exist and are intact, and evaluate the maturity gap between acquirer and target. Consider requiring remediation plans or price adjustments for discovered risks.
Q: How is AI changing the threat landscape?
A: AI enables attackers to scale reconnaissance, craft highly believable social engineering messages, produce audio/video deepfakes, and automate malware generation. Defenders must prioritize identity protection, anomaly detection, layered defenses, and ongoing staff training to reduce susceptibility to AI-enhanced attacks.
Q: What makes a training program effective in a healthcare environment?
A: Effective training is role-based, practical, measured, and engaging. Simulated phishing, scenario-based tabletop exercises, incentives for safe behavior, and inclusion of clinical workflows make training relevant. Leadership involvement and policy reinforcement maintain momentum.
Q: How often should backups and recovery tests be performed?
A: Backup frequency and recovery testing depend on clinical impact and acceptable RTO/RPO. Critical systems should have frequent backups and routine recovery tests (at least quarterly), while lower-impact systems may be tested less frequently. The key is to validate recovery end-to-end, including data integrity and procedural readiness.
Q: When should a healthcare organization hire a CISO or engage a fractional CISO?
A: If the organization lacks internal leadership to consolidate governance, drive risk management, and interface with the board, it should consider a CISO or a fractional CISO. Fractional arrangements provide strategic leadership and program management for organizations that cannot justify a full-time hire.
Appendix: Quick Checklists for Leaders
Executive Quick-Start Checklist (One-Page)
- Assign an executive sponsor for security.
- Define the top three business risks related to patient data.
- Confirm MFA for all administrative access.
- Verify backups are isolated and schedule a recovery test.
- Initiate phishing simulation for staff within 30 days.
- Request a vendor inventory and identify the top 10 vendors by PHI access.
- Schedule a tabletop incident response exercise, including clinical leaders.
Vendor Due Diligence Checklist
- Does the vendor process or store PHI?
- Do contracts include security and breach notification clauses?
- Does the vendor provide SOC 2 or similar attestation?
- Are vendor access accounts time-limited and role-based?
- Is there logging of vendor actions and integration into SIEM if applicable?
Closing Thoughts
Protecting healthcare organizations from cyber threats is both a technical challenge and a leadership challenge. Chris Davenport’s experience underscores a simple truth: security succeeds when it is treated as an enterprise priority, grounded in policy and risk management, enabled by focused controls, and sustained through a culture that values patient safety and operational resilience.
Leaders who act now, aligning governance, shoring up critical controls, building human firewalls, and preparing for AI-driven threats, will be better positioned to protect patients, preserve reputation, and continue delivering care without disruption.